Meningitis is a serious medical condition that occurs when the protective membranes covering the brain and spinal cord—known as the meninges—become inflamed. This inflammation can be triggered by a bacterial, viral, or fungal infection, and in some cases, it can result from non-infectious causes like autoimmune diseases or cancer. Meningitis can affect people of all ages, but infants, young children, and those with weakened immune systems are at greater risk. If not diagnosed and treated quickly, meningitis can cause severe complications, including brain damage, hearing loss, or even death. In this article, we will break down what meningitis is, its causes, symptoms, diagnosis, treatment, and long-term risks.
Understanding the Basics of Meningitis
The human brain and spinal cord are protected by three layers of tissue called the meninges. These layers not only provide cushioning but also serve as a barrier against infection and injury. When harmful agents like bacteria or viruses enter the bloodstream and reach the central nervous system, they can cause inflammation of these membranes, resulting in meningitis.
There are three major types of meningitis based on the cause:
- Bacterial meningitis: The most serious and potentially life-threatening form.
- Viral meningitis: More common and usually less severe.
- Fungal meningitis: Rare and often affects individuals with compromised immune systems.
Each type presents its own set of challenges in diagnosis, treatment, and long-term outcomes.
Bacterial Meningitis: A Medical Emergency
Bacterial meningitis is considered a medical emergency. It progresses quickly and can cause severe damage to the brain and other organs if not treated immediately. Common bacteria that cause meningitis include:
- Neisseria meningitidis (meningococcal)
- Streptococcus pneumoniae (pneumococcal)
- Haemophilus influenzae type b (Hib)
- Listeria monocytogenes
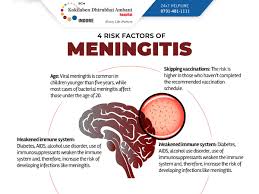
These bacteria can spread through close personal contact, respiratory droplets, or contaminated food. Infants, elderly individuals, and people with weakened immune systems are most at risk.
Symptoms usually appear suddenly and include:
- High fever
- Severe headache
- Stiff neck
- Sensitivity to light
- Nausea and vomiting
- Seizures
- Confusion or difficulty concentrating
In infants, symptoms may include irritability, constant crying, poor feeding, and a bulging soft spot on the head (fontanelle).
Viral Meningitis: Less Severe But Still Serious
Viral meningitis is more common than bacterial but generally less severe. It is often caused by enteroviruses, herpes simplex virus, or the mumps and measles viruses. People with viral meningitis may experience symptoms similar to bacterial meningitis but usually recover on their own without the need for intensive medical treatment.
However, some cases can still lead to complications, especially in young children, older adults, and people with weakened immune systems. Fatigue, memory problems, and light sensitivity may persist for weeks or even months after recovery.
Fungal and Other Types of Meningitis
Fungal meningitis is rare but can be life-threatening. It typically affects people with compromised immune systems, such as those undergoing cancer treatment, people living with HIV/AIDS, or organ transplant recipients. It is usually caused by Cryptococcus or Histoplasma fungi.
Other rare types of meningitis include parasitic and non-infectious forms. Non-infectious meningitis can be caused by autoimmune disorders, certain medications, or brain injuries. Though less common, these forms can still lead to significant health risks and require appropriate medical evaluation and care.
How Meningitis Spreads
The transmission of meningitis largely depends on the underlying cause:
- Bacterial meningitis spreads through coughing, sneezing, or close personal contact such as kissing or sharing utensils.
- Viral meningitis spreads via direct contact with an infected person’s saliva, mucus, or feces.
- Fungal meningitis is not contagious and generally comes from environmental exposure.
College students living in dormitories, military personnel in barracks, and travelers to high-risk areas are more likely to come into contact with meningitis-causing bacteria due to close living quarters and shared facilities.
Complications and Long-Term Risks
If left untreated, meningitis can lead to devastating complications. Some of the most common long-term effects include:
- Hearing loss: Inflammation can damage auditory nerves and lead to partial or total hearing loss.
- Brain damage: Severe infections can cause permanent cognitive impairments.
- Learning disabilities: Especially common in children who survive meningitis.
- Seizures: Scar tissue in the brain can trigger epileptic activity.
- Kidney or adrenal gland failure: Particularly in meningococcal meningitis, which can cause sepsis.
- Limb loss: In severe cases with sepsis, blood flow may be restricted, leading to tissue death and amputation.
Prompt medical attention is crucial. The faster the diagnosis, the better the chance of avoiding these life-altering complications.
Diagnosis and Testing
Because meningitis symptoms overlap with many other conditions, doctors use a combination of tests to confirm a diagnosis:
- Lumbar puncture (spinal tap): The most definitive test. A sample of cerebrospinal fluid (CSF) is collected to check for infection and inflammation.
- Blood tests: To identify bacteria, viruses, or signs of sepsis.
- Imaging (CT or MRI scans): To rule out other conditions like brain abscess or tumors.
A quick and accurate diagnosis is essential because treatment varies widely depending on the type of meningitis.
Treatment Options
Treatment depends on the cause:
- Bacterial meningitis: Requires immediate hospitalization and intravenous antibiotics, and sometimes corticosteroids to reduce inflammation.
- Viral meningitis: Often resolves on its own with supportive care like rest, fluids, and over-the-counter medications.
- Fungal meningitis: Treated with long courses of antifungal medications, often given intravenously.
For all types, early intervention improves outcomes significantly. In bacterial cases, delaying treatment by even a few hours can drastically increase the risk of death or permanent disability.
Prevention: What You Can Do
Preventing meningitis involves a combination of lifestyle habits, awareness, and medical interventions:
1. Vaccination
Vaccines are the most effective way to prevent many forms of meningitis. Recommended vaccines include:
- Meningococcal vaccine
- Pneumococcal vaccine
- Hib (Haemophilus influenzae type b) vaccine
- MMR (measles, mumps, rubella) vaccine
Children should receive these vaccines as part of their routine immunization schedule. Teenagers and college students are also advised to get booster shots, especially before living in communal settings.
2. Hygiene
Simple hygiene practices can reduce the risk of infection:
- Wash hands frequently
- Avoid sharing eating utensils, drinks, and personal items
- Cover your mouth when coughing or sneezing
3. Strengthen Immune System
Maintain a healthy lifestyle with good nutrition, regular exercise, and adequate sleep to support a strong immune response.
4. Awareness While Traveling
If you are visiting areas where meningitis is more common—such as parts of Africa—consult your doctor about necessary vaccinations and precautions.
Living After Meningitis: Recovery and Rehabilitation
Recovery from meningitis can take weeks or months. Physical therapy, occupational therapy, and counseling may be needed to help patients regain lost functions. Children may require academic support if cognitive functions have been affected.
Families of meningitis survivors should be alert to signs of long-term complications and stay in close contact with healthcare providers. Early intervention can make a significant difference in regaining quality of life.
Conclusion: Knowledge Is Your Best Protection
Meningitis is a condition that can escalate rapidly and leave lasting consequences. Understanding its causes, symptoms, and risks is the first step in preventing and managing this potentially deadly disease. With timely diagnosis, effective treatment, and preventive care like vaccination, most people can recover fully and avoid severe outcomes.
Spreading awareness, especially in high-risk communities and among parents of young children, is essential. The more informed we are, the more prepared we become to protect ourselves and our loved ones from the dangerous impact of meningitis.